Not long ago, my Congressman emailed out a poll wherein he asked his constituents what they thought of the Democratic health-care plan. Annoyed that my Congressperson was reducing my thoughts on such a complex topic to a “yes” or “no” radio button, I instead wrote him back, saying in brief that I felt our health-care system desperately needed SOME kind of reform.
A week later I got a thorough response from Congressman Carter (or his form-letter-writing staffer, either way) thanking me for my contribution and outlining why he was against “Obamacare.” He led off with a striking couple of sentences:
America has the highest quality health care in the world. A recent medical study on cancer survivability rates showed that Americans are in a lot better shape than Great Britain, Norway, and the European Union nations, all of which have government run health care. For example, the survival rate for those diagnosed with prostate cancer in European Union countries is only 77%; it is 99% in the U.S. Additionally, all female cases of cancer have a survivability rate of 62.9% in the United States, but only 52.7% in England.
Bam! My notions that health care is automatically and entirely better in the rest of the industrialized world came crashing down. Those are some powerful statistics there; has the eeeeevil US health-care system really got cancer whipped like that?
My research turned up an interesting and complex topic. Take a second to look at this chart, which compares prostate cancer rates around the world…
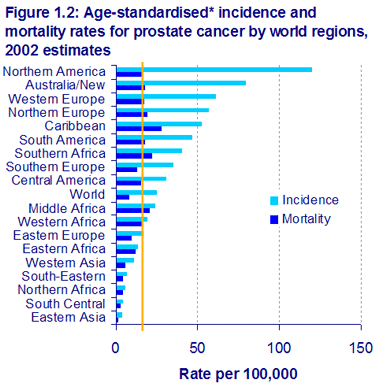
As you can see, we looooove getting prostate cancer over on this continent. Check out the mortality lines, though. If you draw it vertical, you see deaths by prostate cancer are pretty much the same across N. America, Australia, South America, and most of Europe. To restate: if you randomly select 100,000 men in the US, and compare it to any of those other regions, roughly the same number in any group will die of prostate cancer. This appears to be true of other cancer types, as well.
So in short, cancer mortality rates are generally the same. Cancer incidence rates are much much higher here. Dividing one number into the other, you end up with some dramatic differences in survivability rates.
Why the huge disparity? Are American prostates just that much more cancer-prone? Clearly not, just as it’s not likely that so few Asians get prostate cancer. (There might very well be genetic or other factors that cause some disparity, but not to the extent we see in Mr. Bar Graph up there.)
K, so here’s where it gets interesting (if you’re still reading). The US is really, really good at cancer screening. This kinda sucks, though, seeing as we don’t prevent very many more deaths from cancer as other developed regions. This New York Times article lays out the good and the bad of having so much screening, but let me quote a few key portions for you:
Except for a few types of cancer, routine screening has not been proven to reduce the death toll from cancer for people without specific symptoms or risk factors — like a breast lump or a family history of cancer.
Well, as the car mechanic says, there’s your problem. We appear to be spending zillions of dollars screening for cancer—the US spends $4 billion annually on mammograms—when we’re not saving many lives by doing so. Even more interesting: there’s such a thing as too much cancer screening. All those screenings inevitably turn up lumps, tumors, abscesses, and (yes) cancers that aren’t life-threatening. As another example,
A nationwide “Check Your Neck” campaign was intended to highlight screening for thyroid cancer. But thyroid cancer kills 1,600 Americans a year, making it a rare disease [about as deadly as hernias]. And there is no evidence that routine neck exams reduce the risk of dying from thyroid cancer, said Dr. Barnett S. Kramer, the associate director for disease prevention at the National Institutes of Health… Most thyroid cancers are so slow-growing and curable that early detection would not improve their prognosis, he said, while a rarer form of thyroid cancer is so aggressive that a surge in screening would be unlikely to have an impact on the death rate.
But routine screening, he said, does have the potential to do harm because neck exams can find tumors that would not otherwise have required treatment, potentially setting off a cascade of unnecessary events like ultrasounds, needle biopsies in the neck, operations to remove the thyroid and complications like damage to the vocal cords. Meanwhile, Dr. Kramer said, the exams can miss some life-threatening cancers that are not detectable by touch.
To offer ONE MORE quote from the article… you really should just read it…
Dr. Ned Calonge, the chairman of the United States Preventive Services Task Force said, “There are five things that can happen as a result of screening tests, and four of them are bad.” …The one good result of screening, Dr. Calonge said, is identifying a life-threatening form of cancer that actually responds to timely intervention.
The possible bad outcomes, he said, are results that falsely indicate cancer and cause needless anxiety and unnecessary procedures that can lead to complications; that fail to diagnose an existing cancer, which could lull a patient into ignoring real symptoms as the cancer progresses; that detect slow-growing or stable cancers that are not life-threatening and would not otherwise have required treatment; and that detect aggressive life-threatening cancers whose outcome is not changed by early detection.
In other words, cancer screening is useful “only if, on balance, the deaths prevented by treating cancers outweigh the harm done by treatments that are not medically necessary.”
Okay, I hear the objections already: “I would rather be screened too much than not enough.” Well, yes and no. On an individual level, it’s all about how panicky you want to be about your personal health. You can spend a half-hour every morning checking every part of your body for every possible type of cancer, sure. You can also change your socks once an hour to prevent athlete’s foot. But it all seems a bit excessive, no?
On a macro level, it’s a little more serious than needing to wash your socks more often, or being a half-hour late to work. It’s billions of dollars spent locating cancers when not so many people are going to be affected by it. Don’t get me wrong, cancer is a scary-ass thing… it’s the second-leading cause of death in this country. But, weird as it sounds, screening for cancer appears to be even more of a public health problem.
That’s my take on it, anyway.
I’m evidence of this over-screening. I have an enlarged thyroid, and to “keep an eye on it” I’m supposed to get an ultrasound once a year. Despite the fact that I have no symptoms or problems. Good thing I’ve got generous employer-paid health care, right? But what if I’m eating into my lifetime cap everytime I get one of these scans that show I’m still a-ok? Of course, nothing comes out of my pocket right now, so I’m not motivated to say thanks but no thanks to a free ultrasound that I don’t need. (I’ve got a lot of other examples involving multiple MRIs, but I won’t bore you…)
Good stuff Kevin, keep going!
While I see what you are trying to say, I must object. My maternal grandmother is not alive today because her HMO refused to test her for ovarian cancer. She went in knowing that there was something wrong. They told her that she had an ulcer and would not test her for cancer because it is too expensive. She continued to complain about her poor health and they still refused to give her the test. You see, she was older, lived alone, and they thought no one would care if she died. I won’t go into all the details because it is a very long story. However I will say that when she came to visit us, her abdomen was so swollen that she looked like she was pregnant. Her doctor had told her it was because of the altitude of Colorado, where she lived at the time. We took her to a hospital here and they diagnosed her with stage 4 ovarian cancer. My grandmother died for only one reason, because it was too expensive to treat her.
She was not a statistic. She was my grandmother and I loved her. I do not want to die like she did, just because it is too expensive to do the test that will save my life.
@Christine: Your grandmother suffered not just from ovarian cancer but from an insurance company that was more concerned with the bottom line than health and a doctor that just plain didn’t care.
Sounds like a great argument for health insurance reform.
@Tyler: I agree that there should be reform, but not the kind Obama is proposing.